|
ORIGINAL ARTICLE |
https://doi.org/10.5005/jp-journals-10080-1548
|
Growth Deceleration for Limb Length Discrepancy: Tension Band Plates Followed to Maturity
1–5Department of Orthopedics, University of Utah, Salt Lake City, Utah, United States of America
Corresponding Author: Peter Stevens, Department of Orthopedics, University of Utah, Salt Lake City, Utah, United States of America, Phone: +8013303656, e-mail: peter.stevens@mac.com
How to cite this article: Stevens P, Desperes M, McClure PK, et al. Growth Deceleration for Limb Length Discrepancy: Tension Band Plates Followed to Maturity. Strategies Trauma Limb Reconstr 2022;17(1):26–31.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Objective: There are several alternative methods for accomplishing epiphysiodesis of the longer limb to address limb length discrepancy (LLD). Consensus is lacking regarding the optimal timing of the intervention and which method is most efficacious. We reviewed a large group of patients with anisomelia treated by tethering with tension band plates (TBP) and who had attained skeletal maturity. We discuss our preferred timing and technique while noting the complications and how they were managed.
Materials and methods: With IRB approval, we reviewed 66 subjects including 32 boys and 34 girls, ranging in age from 3 to 16.6 years at the time of physeal tethering, who were destined to have between 2 and 9 cm LLD at maturity. Inclusion criteria were: (1) at least 1 year of predicted growth at the time of tethering; (2) minimum 18-month follow-up and (3) minimum Risser stage 1 (R1) in the last radiologic study. There were 35 distal femoral, 25 pan genu and five proximal tibial procedures. Patients were seen bi-annually with weight-bearing full-length radiographs to ascertain neutral alignment and assess limb lengths.
Results: We defined a successful outcome to be <1.5 cm of residual discrepancy. Iatrogenic mechanical axis deviation, observed in nine patients (five varus and four valgus), was successfully managed by repositioning the implants. While the under-corrected patients presented too late to achieve equalization, they benefited from partial improvement. Due to lack of timely follow-up, one patient over-corrected by 2 cm and had a femoral shortening at the time of correcting contralateral femoral anteversion. One patient required a distal femoral osteotomy to correct recurvatum at maturity.
Conclusion: Properly timed and executed, TBP is an efficacious and reversible means of growth deceleration, rather than growth arrest, that may be applied in a wide age range of patients with modest anisomelia regardless of aetiology. This method offers potential advantages over purportedly rapid and definitive techniques such as percutaneous epiphysiodesis (PE) or percutaneous epiphysiodesis with transphyseal screws (PETS).
Level of evidence: Level III. Retrospective series without controls.
Keywords: Anisomelia, Epiphysiodesis, Limb length inequality, Tension band plating.
INTRODUCTION
Epiphysiodesis of the longer limb is warranted when a limb length discrepancy (LLD) is projected to reach between 2 and 5 cm at maturity. Popular growth arrest techniques include percutaneous epiphysiodeses (PE) that is permanent or with using transphyseal screws (PETS) that has not been proven to be predictably reversible. Both methods require serial calculations of growth remaining to determine the ideal time for growth arrest. Unfortunately, each of these calculation methods has inherent inaccuracies that may result in over- or under-correction of the discrepancy. This potential source of error may be averted by opting for a reversible technique of growth deceleration which employs an extra-periosteal tension band plate (TBP) to tether each side of the physis. As the intent is to restrain rather than arrest the physis, precise calculations of optimal timing are obviated and this permits earlier intervention when indicated. Subsequent growth reactivation (within 2 years) may be practiced, if needed. The purpose of this study was to document the efficacy of TBP and to discuss its potential benefits and advantages over PE and PETS.
MATERIALS AND METHODS
This is a retrospective, IRB approved, review of the patients we treated with TBP between 2005 and 2017. We included patients with (1) predicted discrepancy of 2–9 cm at maturity; (2) minimum of 1 year of predicted growth remaining at the time of epiphysiodesis; (3) minimum 18-month follow-up and (4) minimum Risser stage I (R1) at the last radiologic study, reflecting impending skeletal maturity. We excluded patients with previous growth modulation history for coronal deformity treatment or insufficient radiologic follow-up or both. There were 66 eligible subjects, including 32 boys and 34 girls, ranging in age from 3 to 16.6 years old at the time of plate epiphysiodesis. The predominant aetiology was idiopathic. Physeal restraint with TBP included 35 distal femoral, 26 pan genu and 5 proximal tibial procedures.
Assessment
For the clinical assessment, we placed a block under the foot of the shorter limb to level the iliac crests and estimate the relative LLD in the standing position. The same block was then used under the short limb to confirm the measurement on a teleroentgenogram. This method includes the contribution of the ileum and the foot to the overall discrepancy. We did not utilise supine CT scanograms due to their multiple shortcomings.1 Specifically, they are not obtained with the patient weight-bearing and do not demonstrate diaphyseal deformities or the mechanical axis. These scanograms do not include the foot and the pelvis, potentially underestimating the aggregate discrepancy. All images were used for measurement; the pre-operative vs final discrepancy, limb segment disparities and the mechanical axis were noted. Iatrogenic intra-articular deformity of the tibia was looked for as well.
Timing
The Moseley Straight-Line Graph or the Multiplier Method each requires meticulous, serial imaging and calculations to determine the optimum timing of intervention. The same would be required for the Metaizeau PETS method of epiphysiodesis which would not, as it may not be reversible, suit younger patients. For adolescents, we used the White-Menelaus technique of calculating growth remaining. This method was compatible with our strategy of reversible growth deceleration. Our preferred timing for physeal deceleration is to perform this elective procedure as soon as the discrepancy reached 2 cm or at least a year earlier than the time if practicing the Phemister epiphysiodesis, PE or Blount stapling techniques. In adolescent patients we obtained a hand film to estimate skeletal age, advising parents that at least 1 year of remaining growth was necessary to justify the recommended surgery. The White-Menelaus method is predicated upon the estimate of 9 mm of distal femoral and 6 mm of proximal tibial growth per year, with girls reaching skeletal maturity at age 14 and boys at age 16 years2–4 (Fig. 1). Mindful of body segment proportions or limited time remaining for growth or both, we employed pan genu plates when deemed appropriate.
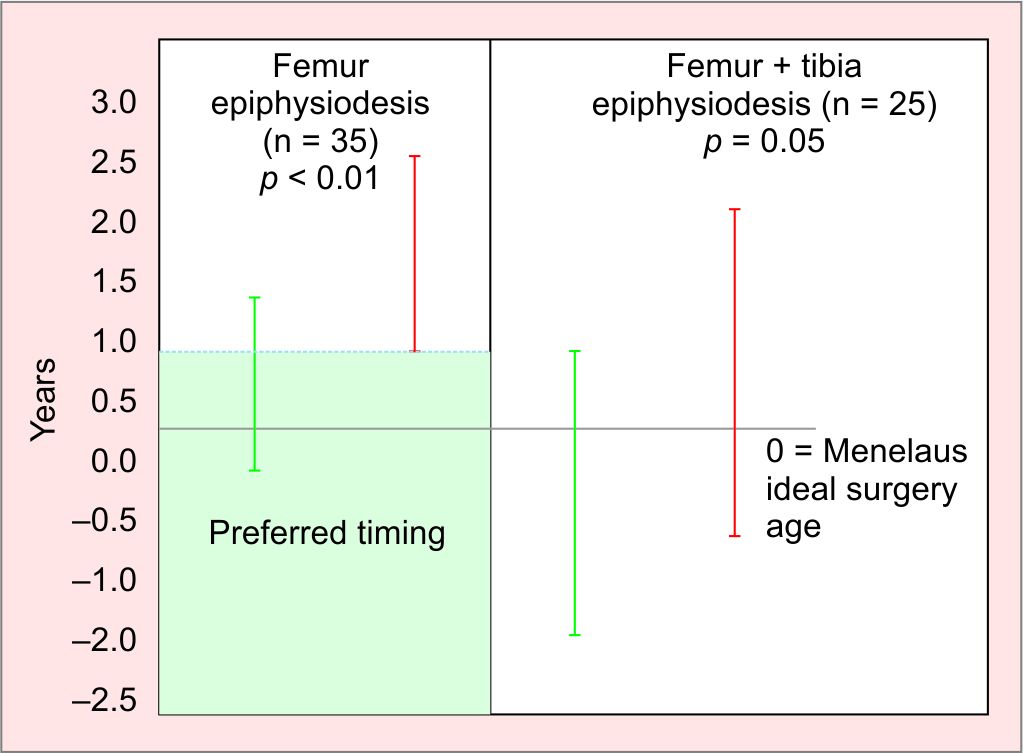
Fig. 1: Physeal tethering is reversible, early intervention is preferable (green). This accommodates any lag time in the effect
Technique
The surgery was performed on an outpatient basis. Under tourniquet control, a single extra-periosteal plate was placed medially and laterally for a given physis. We did not employ dual or quad plates. The fibula was not addressed unless it was judged to be unduly prominent, which was not an issue encountered in this series. We recommend screws that are 32 mm, or longer, on the premise that they are less likely to lose purchase. This may mitigate against valgus or varus drift. A subtle, but important, variation on technique that evolved from the observation that if the screws are placed parallel to each other at the outset, they will diverge over time producing an undesirable lag period before the physis is effectively restrained. Recognizing this phenomenon, we place the screws in a divergent pattern from the outset in order to avoid this undesirable delay (Fig. 2).

Fig. 2A and B: (A) When the screws are placed in a parallel pattern, there may be a latency period of continued physeal growth. This is manifest as gradual divergence of the screws +/1 bending, shown here; (B) By diverging the screws at the outset, they are unlikely to bend and the lag time is reduced. Conceptually, the risk of producing an intra-articular deformity is also mitigated
Postoperatively, patients were permitted to be full weight-bearing and encouraged to resume activities as tolerated. At 1-month after surgery, if a given patient was unable to flex the knee to at least 90°, then physical therapy was prescribed; this was required in less than 10% of patients. Routine follow-up was conducted at 6-month intervals with a full-length standing AP radiograph to measure the remaining discrepancy and detect any drift of the mechanical axis.
At maturity or upon achieving the desired correction, the plates were removed. However, for a patient who has reached maturity and has no discomfort from the implants, these may be left in situ.
Statistical Analysis
Student’s t-test was used to compare the means of the continuous variables with normal distributions stratified by correction (chronological age, BMI, predicted age and surgical date). The Wilcoxon rank-sum test was used to compare the ranks of the non-normally distributed continuous data stratified by correction (predicted discrepancy, screw divergence angle). The Chi-squared test was used to determine if there was a relationship between the categorical variables and correction (sex, operated segments, diagnostic category, screw angle >10° and bone age). To determine if the reactivation rates were significantly different, we performed a 1-sample Wilcoxon signed rank test. We considered p-values less than 0.05 to be statistically significant. The output for this paper was generated using SAS software, version 9.4 (SAS Institute, Cary, North Carolina).
RESULTS
We defined a successful outcome as an LLD equal or less than 1.5 cm at skeletal maturity; 38 patients met these criteria. While the remaining 28 did not achieve that threshold, an improvement had occurred although under-corrected. Prior to surgery we had identified that the more mature adolescents would not have sufficient growth remaining to attain full correction. Despite this information being shared to parents, they had elected to proceed with TBP in order to reduce the discrepancy at maturity.
The mean age at surgery was younger for patients who did achieve adequate correction compared to those who did not (12.3 ± 1.6 and 13.3 ± 1.5, respectively; p = 0.01). This difference persisted in female patients but not in male patients. Patients who failed to achieve correction were more likely to be closer to skeletal maturity or to have larger predicted discrepancies; 35.0 mm (IQR 26.9, 40.8) compared to 29.0 mm for those who achieved correction (IQR 22.0, 35.2). The difference in predicted discrepancy between the corrected and under-corrected groups failed to reach statistical significance, p = 0.06, but is still notable. Bone age data were available for a higher percentage of under-corrected patients (32.1% vs 2.7%, p = 0.001). This reflects our practice to employ the White-Menelaus method to forecast remaining growth in adolescent patients.
For under-corrected patients, the chronological age at surgery was higher than the Menelaus’ prediction (1.1 ± 1.3); for corrected patients, the difference between chronological age at surgery and the Menelaus’ prediction was very small (0.1 ± 1.2). The difference in age discrepancy between the corrected and under-corrected groups was statistically significant (p = 0.002). Patients who became under-corrected and who received treatment for the femur only had the largest difference between predicted age and surgical age (1.6 ± 0.9). This age discrepancy was significantly larger than the age discrepancy for corrected patients (0.4 ± 0.8, p = 0.0003). In patients who had both femur and tibia operated on, the chronological age at surgery was younger on average than the Menelaus’ prediction (−0.6 ± 1.3) for corrected patients and older for under-corrected (0.5 ± 1.5). While this difference failed to reach statistical significance, the difference is notable (p = 0.05). There were insufficient patients who had the tibia treated only to assess the relationship between age discrepancy and achievement of correction.
For immature patients who achieved equal limb lengths, the hardware was removed. No premature physeal closure was observed. The average follow-up after hardware removal was 13.0 months (IQR 8.0, 30.0). Of the 24 patients with reactivation rate data (18 femur, 6 tibia), there were 3 femur and 2 tibia in patients with 0 growth after reactivation. The median reactivation rate for the femur was 0.98 (IQR 0.50, 1.07, p = 0.20) and for tibia it was 1.01 (0.69, 1.36, p = 0.88. Under-corrected patients with a parallel or divergent screw angle were on average a year older than the Menelaus’ prediction at the time of surgery (1.2 ± 1.6 and 1.1 ± 1.3, respectively). The age discrepancies between corrected and under-corrected patients with divergent screw angles were significantly different (p = 0.001).
There were no perioperative infections. In a single patient, two of the screw heads sheared off at the time of implant removal. We did not attempt to remove the embedded screw shanks. This has caused no postoperative sequelae and had no impact upon the successful outcome. There were no other patients with broken screws or plates. We did not identify BMI as a risk factor for hardware failure in this series of LLD patients. One patient with gigantism due to an extensive congenital haemangioma developed subsequent bilateral genu valgum. This was treated by serial guided growth and equal limb lengths were achieved. At maturity he was symptomatic secondary to genu recurvatum, which was not attributed to plate position, and required a supracondylar flexion osteotomy. One patient with LLD as a sequela of treatment for developmental dysplasia of the hip (DDH) developed 2 cm over-correction following guided growth. This occurred due to a lack of timely follow-up. The discrepancy was resolved at the time of a contralateral rotational osteotomy to correct 30° of femoral anteversion by concomitant shortening.
There was a deviation of the mechanical axis in nine patients. Iatrogenic genu varum (zone −2) occurred in five and genu valgum (zone +2) in four subjects. This was successfully managed by removing the plate (or metaphyseal screw) from the concave side of the deformity, allowing the mechanical axis to revert to neutral and re-implanting the hardware. Pursuing this strategy, no salvage osteotomies have been required for iatrogenic coronal plane deformity.
DISCUSSION
The concept of epiphysiodesis to correct modest LLD was first introduced by Phemister in 1933.5 Blount introduced the concept of physeal stapling soon afterwards.6 These two methods (Fig. 3) were practiced widely for decades. Subsequent to the introduction of fluoroscopy, the Phemister technique was refined to facilitate percutaneous physeal ablation.7 This became popular and had acceptable results. However, the principal disadvantage of PE is the difficulty in determining the exact timing for intervention along with the inherent permanent and irreversible nature of the result, leading to potential over- or under-correction (Fig. 3). In addition, an asymmetrical arrest may produce an iatrogenic angular deformity; the only salvage is a corrective osteotomy. More recently, Metaizeau popularised the method of percutaneous epiphysiodesis using transphyseal screws (PETS).8 The traversing across the physis with a pair of 6.5 diameter screws is unappealing and may pose a risk of physeal closure following hardware removal. Hence, typical PETS series reported are in adolescent patients.
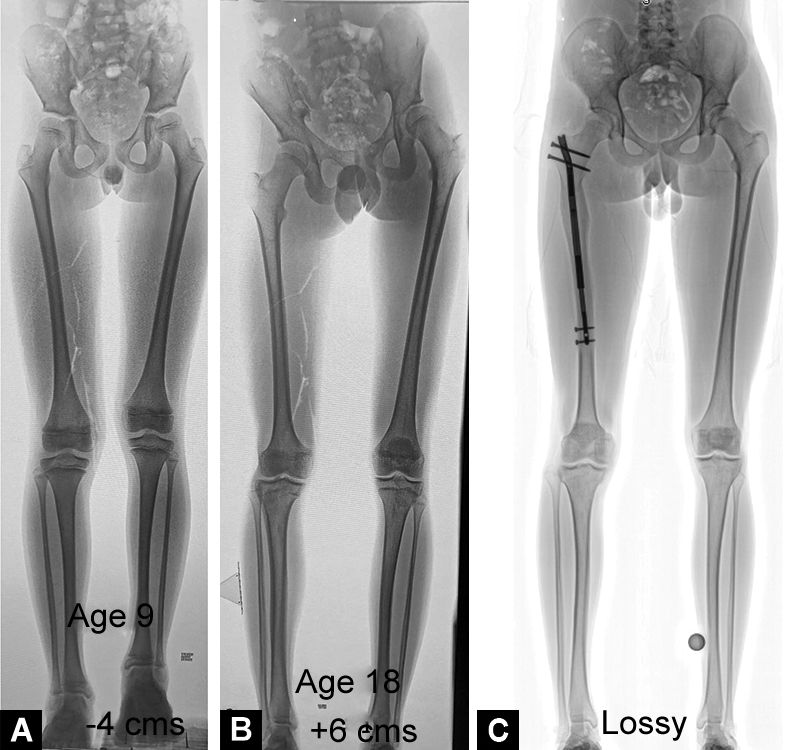
Fig. 3A to C: (A) This boy presented at age 9 with 4 cm LLD, attributed to Beckwith-Wiedeman syndrome and causing progressive overgrowth on the right. Pan genu-guided growth was recommended; (B) Instead, the family chose to wait and eventually, at age 12, he underwent ‘definitive’ treatment elsewhere, comprising pan genu PE. This miscalculation resulted in gross over-correction, with an LLD at maturity = 6 cm (now shorter on the right); (C) This iatrogenic deformity was eventually remedied by femoral lengthening with a PRECICE intramedullary rod
As each of these ablative or compressive methods may produce a permanent arrest of the physis, intentionally or otherwise, these must be timed precisely. The Green Anderson tables were the sole planning resource available for nearly 40 years.9 The Moseley Straight-Line Graph Method was employed for nearly two decades.10 This required serial scanograms and hand radiographs to estimate skeletal growth remaining. Introduced in 2000, the Multiplier Method, running in a smart phone application, has been popularised and is very convenient to use.11 This method includes the femur and tibia but not the ileum and foot and may thus underestimate some discrepancies. Each of these predictive methods has potential inaccuracies, making precise timing elusive. None has been proven to be superior to the White-Menelaus method for calculating timing.12–15
This inability to produce accurate timings for interventions supports the concept of reversible growth deceleration as a means of addressing limb length inequality. While extra-physeal stapling is theoretically reversible and was popular for several decades, problems with staple breakage or migration resulted in unplanned revision surgery and sometimes untoward outcomes. Observed spreading of reinforced staple prongs prompted the use of 2–3 staples on each side of the physis. Staples have largely been abandoned in favour of bilateral plates that are more resilient and secure.16 Tension band plates have been well-accepted for the correction of angular deformities. However, the use of a pair of plates for the management of anisomelia has been the subject of controversy. Recent publications have suggested that this technique is ineffective and best avoided. One study compared tension band plates with the Metaizeau technique (PETS) at intervals of 6 and 18 months post implantation and concluded that the latter was faster and thus preferred.17 It is incorrect to assume that extra-periosteal plates are just another means of producing immediate arrest of the physis in the same manner as two 6.5 mm cancellous screws placed across.18 Other authors have concluded that permanent techniques such as percutaneous epiphysiodesis (PE) are more rapid and “powerful” and therefore are “definitive”.19–22 In these manuscripts, several of the case illustrations of TBP demonstrate the technical error of inserting parallel screws. Due to the lag effect, this could explain why they noted slower correction compared to PE or PETS, leading to an erroneous criticism of the technique. This common error in TBP technique was revealed in subsequent letters to the editors.23,24 Other investigators have documented equivalent efficacy amongst each of the currently popular techniques.25
The preferred timing of the techniques that violate the physis, including PETS and PE, is different to that when using extra-periosteal tethering. The intent of applying dual 8-plates is to reversibly decelerate rather than arrest the physis. This obviates the need to time the intervention precisely and supports the wide applicable age range (as young as 3 years of age) and versatility of this method. We recommend TBP when the LLD reaches 2 cm, regardless of age. The Menelaus method is our preferred choice and intervention is planned a year sooner than if carried out with permanent PE. The more mature patients require at least a year of predicted growth remaining to benefit from epiphysiodesis by any method.
Based upon personal communication between Phemister and Blount, but without corroborating evidence, there is a prevailing belief that if a given physis is restrained for over 2 years it may cease to grow.6 This precaution has been respected and practiced for decades but not substantiated in a literature search. Mindful of this concern, the plates or just the metaphyseal screws should be removed within 2 years of growth restraint to prevent premature closure. If additional length adjustment is warranted, they may be reinserted after a period of 6 months, effecting a serial deceleration (Fig. 4). Iatrogenic angular deformity may readily be managed by timely removal or repositioning of implants.

Fig. 4A and B: This 3-year-old presented with symptomatic LLD = 5 cm and a predicted discrepancy at maturity of 9.9 cm. Pan genu-guided growth was commenced at age 3 and repeated at 2 years intervals, removing metaphyseal screws for up to 6 months, to allow physeal reactivation, then reinserting. There is no resultant pagoda deformity of the tibia
A concern expressed by some observers is the potential for dual plates to cause iatrogenic intra-articular deformity of the tibia, namely, ‘pagoda tibia’.22 This effect was not observed in this cohort and we postulate that this may be avoided by adopting practice of placing longer screws in a divergent pattern.
CONCLUSION
This series represents a comparatively large collection of patients who underwent guided growth for LLD and were followed to skeletal maturity. Premature physeal closure did not occur. The following observations were made: (1) growth deceleration with TBP is effective; (2) it is reversible and, therefore, applicable in younger patients who are symptomatic due to LLD greater than or equal to 2 cm; (3) a divergent placement of the screws is recommended because it averts a latency period. This also mitigates against bending of screws potentially averting the production of intra-articular deformity; (4) TBP is recommended at least a year sooner than typically advocated for other methods of epiphysiodesis; (5) in adolescents, the White-Menelaus method is well suited for planning for this method of epiphysiodesis. While subtle and more anticipatory as compared to permanent methods, TBP deserves a place in the current armamentarium of treatment modalities for LLD.
REFERENCES
1. Machen MS, Stevens PM. Should full-length standing anteroposterior radiographs replace the scanogram for measurement of limb length discrepancy? J Pediatr Orthop (B) 2005;14(1):30–37. DOI: 10.1097/01202412-200501000-00005.
2. White JW, Stubbins SG. Growth arrest for equalizing leg lengths. Journal of the American Medical Association 1944;126(18):1146–1149. DOI: 10.1001/jama.1944.02850530024006.
3. Menelaus MB. Correction of leg length discrepancy by epiphyseal arrest. J Bone Joint Surg (B) 1966;48(2):336–339. PMID: 5937598.
4. Westh R, Menelaus M. A simple calculation for the timing of epiphyseal arrest: a further report. J Bone Joint Surg 1981;63(B):117–119. DOI: 10.1302/0301-620X.63B1.7204464.
5. Phemister D. Operative arrestment of longitudinal growth of bones in the treatment of deformities. J Bone Joint Surg 1933;15(1):1–15.
6. Blount WP, Clarke GR. Control of bone growth by epiphyseal stapling. J Bone Joint Surg 1949;31(A3):464–478. PMID: 18153890.
7. Bowen JR, Johnson WJ. Percutaneous epiphysiodesis. Clin Orthop Relat R 1984;190:170–173. PMID: 6488627.
8. Metaizeau JP, Wong-Chung MC, Bertrand H, et al. Percutaneous epiphysiodesis using transphyseal screws (PETS). J Pediatr Orthop 1998;18(3):363–369. PMID: 9600565.
9. Green W, Anderson M. Skeletal age and the control of bone growth. Instr Lect Am Acad Orthop Surg 1960;17:199–217. PMID: 13708221.
10. Moseley C. A straight-line graph for leg length discrepancies. Clin Orthop Relat R 1978;136:33–40. PMID: 215368.
11. Paley D, Bhave A, Herzenberg JE, et al. Multiplier method for predicting limb-length discrepancy. J Bone Joint Surg 2000;82(10):1432–1446. DOI: 10.2106/00004623-200010000-00010.
12. Makarov MR, Jackson TJ, Smith CM, et al. Timing of epiphysiodesis to correct leg-length discrepancy: a comparison of prediction methods. J Bone Joint Surg 2018;100(14):1217–1222. DOI: 10.2106/JBJS.17.01380.
13. Song H, Eun-Seok C, Seok M, et al. Percutaneous epiphysiodesis using transphyseal screws in the management of leg length discrepancy: optimal operation timing and techniques to avoid complication. J Pediatr Orthop 2015;35(1):89–93. DOI: 10.1097/BPO.0000000000000214.
14. Dimeglio A, Kelly P. Lower-limb growth: how predictable are predictions? J Child Orthop 2008;2(6):407–415. DOI: 10.1007/s11832-008-0119-8.
15. Birch JG, Makarov MA, Jackson TJ, et al. Comparison of Anderson-Green graphs and white-menelaus predictions of growth remaining in the distal femoral and proximal tibial physes. J Bone Joint Surg Am 2019;5;101(11):1016–1022. DOI: 10.2106/JBJS.18.01226.
16. Lee SC, Shim JS, Seo SW, et al. The accuracy of current methods in determining the timing of epiphysiodesis. J Bone Joint Surg 1995;7:993–1000. DOI: 10.1302/0301-620X.95B7.30803.
17. Pendleton A, Stevens PM, Hung M. Guided growth for the treatment of moderate leg-length discrepancy. Orthopedics 2013;36(5):e575–e580. DOI: 10.3928/01477447-20130426-18.
18. Gaumetou E, Mallet C, Souchet P, et al. Poor efficiency of eight-plates in the treatment of lower limb length discrepancy. J Pediatr Orthop 2016;37(7):715–719. DOI: 10.1097/BPO.0000000000000518.
19. Bayhan I, Karatas A, Rogers K, et al. Comparing percutaneous epiphysiodesis for the treatment of limb length discrepancy. J Pediatr Orthop 2017;37(5):323–327. DOI: 10.1097/BPO.0000000000000647.
20. Borbas P, Agten C, Rosskopf A, et al. Guided growth with tension band plate or definitive epiphysiodesis for treatment of limb length discrepancy? J Orthop Surg Res 2019;14(1):99. DOI: 10.1186/s13018-019-1139-4.
21. Lauge-Pedersen H, Hagglund G. Eight plate should not be used for leg length discrepancy. J Child Orthop 2013;7(4):285–288. DOI: 10.1007/s11832-013-0506-7.
22. Stewart D, Cheema A, Szalay E. Dual 8-plate technique is not as effective as ablation for epiphysiodesis about the knee. J Pediatr Orthop 2013;33(8):843–846. DOI: 10.1097/BPO.0b013e3182a11d23.
23. Stevens PM. Invalid comparison between methods of epiphysiodesis. J Pediatr Orthop 2018;38(1):e29–e30. DOI: 10.1097/BPO.0000000000001020.
24. Kaymaz B, Komurcu E. Comment on the article “Dual 8-plate technique is not as effective as ablation for epiphysiodesis about the knee” by Stewart et al. J Pediatr Orthop 2014;34(8):e67. DOI: 10.1097/BPO.0000000000000314.
25. Lykissas M, Jain V, Manickam V, et al. Guided growth for the treatment of limb length discrepancy: a comparative study of the three most commonly used surgical techniques. J Pediatr Orthop (B) 2013;22(4):311–317. DOI: 10.1097/BPB.0b013e32836132f0.
________________________
© Jaypee Brothers Medical Publishers. 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution-Non Commercial-share alike license (https://creativecommons.org/licenses/by-nc-sa/4.0/) which permits unrestricted distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. If you remix, transform, or build upon the material, you must distribute your contributions under the same license as original. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.